When this Filipina Pushed Back, All International Nurses Got a Fair Deal
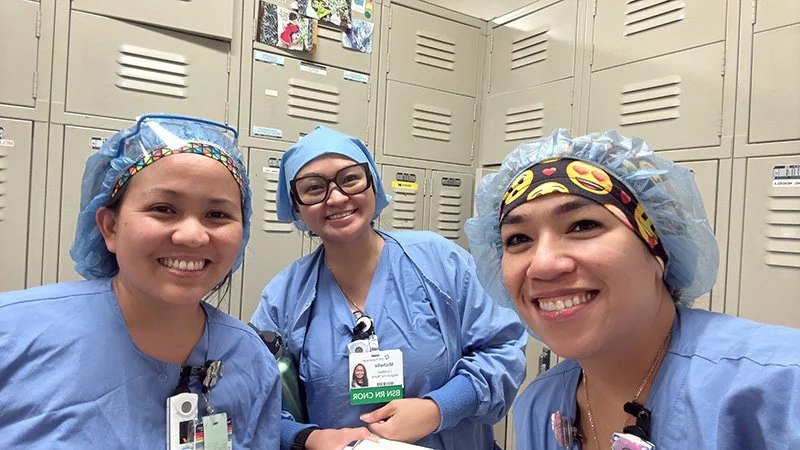
/Kathleen jabasa (right) with operating nurse colleagues Michelle Abenoja, left, and Carolyn Catindig, center, after their shift. (Photo courtesy of Kat Jabasa)
Led by Kathleen Jabasa, an operating room nurse and grievance officer with the Washington State Nurses Association (WSNA), nurses at St. Joseph Medical Center successfully pressed management to revoke an unfair policy, securing full credit for international nurses’ overseas experience. WSNA is their union.
“I’m standing here today not just for myself but for every international nurse who ever felt unheard or undervalued,” stated Nurse Jabasa on June 9, 2025, at the ceremony where she accepted the annual WSNA Health Equity Award. “The victory is more than financial. It’s a restoration of dignity, our pride, and our rightful place in the field of nursing.”
Jabasa, 46, and her nurse colleagues sought to eradicate a bias that economically harmed immigrant nurses predominantly from the Philippines, Ghana, India, and other underdeveloped nations whose families depend on remittances from relatives in the U.S.
When determining seniority and compensation, the 337-bed hospital, fondly known as “St. Joe’s,” calculated an international nurse’s prior experience with a formula of a half-year for every year of work outside of the United States and Canada.
“I have a total of 25 years of nursing experience,” Jabasa summed up her nursing background of 15 years in the Philippines and 10 years in Washington State and Arizona since she joined St. Joe’s in 2019.
She earned her bachelor’s and master’s degrees in nursing from Cebu Doctors University in Cebu, Philippines. Most of her nursing career in the Philippines was spent in patient care and academics. “I served as a Clinical Educator at Cebu Doctors University, which is among the top 10 universities of nursing in the Philippines.”
To critics of overseas education, she replies, “I was a clinical instructor for a lot of students who came to the United States. We use the same books as American students.
“We had lots of sons and daughters of people in the U.S. who sent their children back to the Philippines to study nursing,” she recalls. “We incorporated into our curriculum preparation for the National Council Licensure Examination, so that our students could practice in the U.S.”
Kathleen Jabasa with her sons Andrei, left, Josh, right, and husband, Aaron. (Photo courtesy of Kat Jabasa)
Righting a Wrong
Jabasa quarterbacked a bargaining team of 11 nurses in grievance sessions and negotiations with hospital administrators. “Let’s say you’ve been a nurse for 15 years with 10 years of that experience in the Philippines and five years in the U.S. So, you will basically receive credit for five years in the Philippines and five years in the U.S.” What this means, she says, “You’re missing out on five years of experience. You will be placed at a Step 10 for 10 years as a nurse. That affects your pay.”
By a reduced valuation of work experience, hospital administrators implied that the responsibilities of nurses in the Philippines were inferior to those in America. “Our practice in the Philippines is at par with any practice here. In fact, I believe our nursing students can do more because there aren’t a lot of medical lawsuits in the Philippines,” she compares hospital systems.
“Here,” she observes, “it’s more restrictive. If you have students that follow you in the hospital, they cannot do much of anything. In the Philippines I remember myself as a student already assisting doctors in delivering babies. I was assisting doctors in surgeries. That was before I finished my bachelor’s degree in nursing at age 19.”
She appreciated that St. Joe’s physicians supported international nurses in changing hospital policy. Nothing could replace the humanity of Filipino nurses during a stressful period in a patient’s life. Jabasa has always empathized with surgical patients who were about to undergo traumatic procedures.
“We fight the same fight to protect our patients’ rights. This is what I always tell my patients when we’re about to put them to sleep.” She assures them, “I know you’re going to sleep, but rest assured, nothing is going to happen to you because I will be your eyes and your voice while you are asleep.”
Jabasa had to also conquer an impeding attitude among fellow Filipinas. “A lot of us Filipinas are just thankful to be in the U.S. Everything is fine with us because we’re still earning more than if we were in the Philippines.” She concedes, “It’s always an attitude of gratitude.”
Kathleen Jabasa (center), and colleagues at a summer bonding experience at Owens Beach in Tacoma. (Photo courtesy of Kat Jabasa)
Times They Are a-Changing
St. Joe’s was founded by the Sisters of St. Francis of Philadelphia in 1891. The average age of the remaining 270 members of sisters in the congregation is 84. Their affiliation with St. Joe’s ended in 1996 when the hospital joined Catholic Healthcare Initiatives (CHI) Franciscan system in 1996. In 2021, CHI Franciscan merged with Virginia Mason to form Virginia Mason Franciscan Health (VMFH), which is under the nonprofit CommonSpirit health system.
At about the time Jabasa was ready to leave her position at a dialysis center, St. Joe’s was one of two hospitals that offered her work. The second opportunity came from MultiCare health system.
“St. Joseph’s was still part of Catholic Health Initiatives Franciscan. I assumed it was a Catholic hospital because of the name Catholic Health Initiatives. I also assumed I had the same Catholic values and shared the same purpose,” explains Jabasa.
You won’t find a habit on the head or Roman collar around the neck of anyone on the CommonSpirit Board, in VMFH leadership or in St. Joe’s President’s suite. Secular priorities, such as revenue goals, can lead to trouble not unlike recent revelations in the St. Providence Health System.
Workers Are the Conscience
Like most hierarchical organizations outside of the Francis I and Leo XIV Vatican, the relationships between the workers on the ground can greatly influence progress in accomplishing the Lord’s mission. Jabsa is happy that she chose St. Joe’s because of her daily encounters in the hallways, in the clinics, on the floor, and in operating rooms.
Her connection with the hospital started with a propitious encounter with a senior Filipina nurse during her stay at St. Joe’s for a gallbladder operation. “The nurse who was taking care of me heard I was Filipina. She said, ‘I’m retiring soon. Maybe you should apply to take my job.” Jabasa recounted, “I was in surgery on Saturday. On Sunday, I attended Mass in the hospital chapel. I was able to honor my religious obligation. Our values aligned.
“But a lot of things have changed,” she admits without giving specifics these six years after she joined St. Joe’s.
Kathleen Jabasa, MSN, RN, accepts the 2025 Washington State Nurses Association Health Equity Award, which recognizes excellence in ethics and the advancement of health equity in nursing. Jabasa led the fight at St. Joseph Medical Center in Tacoma, Washington, to treat nurses trained outside of the United States and Canada, as equals in terms of experience. (Photo by WSNA)
A Deadly Disease Hits Close to Home
The pandemic was a historic crisis that wreaked havoc early in her tenure at St. Joe’s. “It was the hardest time. I’ve been trying to block out much of this experience. Scary things happened to me during the pandemic.”
Jabasa is among the many Pacific Northwest healthcare workers who vividly recall the January 15, 2020, COVID case that started a frenzy on the global stage. She describes the early days of the disease known as corona virus of 2019. “The first COVID patient was in Washington.” Of the danger of being first, she says, “Anyone in Washington could have been infected. And at that point, we didn’t have enough N95 masks.”
Hospital administrators thought they had picked the right approach for rationing masks, but it wasn’t right for the early stage of the disease’s transmission. “We were allowed to use N95 masks if our patient tested positive. We were saving everything when I was assigned to this one patient with COVID symptoms who hadn’t tested positive. If any patient were going to test positive, it was this one. My manager at the time said, ‘Well according to our policy, we can’t give you an N95 (mask) because this patient has not tested positive.’”
Jabasa, 46, and her nurse colleagues sought to eradicate a bias that economically harmed immigrant nurses predominantly from the Philippines, Ghana, India, and other underdeveloped nations.
Nurse Jabasa discussed a distinctly Filipino trait that guided her decision. “I had the mentality of a lot of Filipinos. Someone has to take care of this patient. If that’s me, so be it.” She resolves, “I’m going to take care of this patient. If it’s not my time, God will not take me.
“I’m glad I did not test positive then, though I did get COVID twice since then.” She adds, “The pandemic scared me, but it also strengthened my faith in God.”
Ever since the COVID pandemic, Jabasa has been spurred on by an overt characteristic of her Filipina nature. “When we come into work, people ask us, ‘Why are you always smiling? I’m like, why not? Should I be crying?”
As if to put her capacity to smile under conditions that are as severe as pandemic times, she relates, “This is a trauma center. Patients come in with stab wounds, they have impact injuries like brain trauma and fractures due to car accidents, falls and various collisions. Some patients doubt they will survive. But we’re nurses. We’re there to hold their hand and say, ‘Everything’s going to be OK. We got you.’”
Anthony Maddela is the son of Philippine immigrants who met in post-WWII Seattle. He is one of four siblings born in Seattle. His youngest sister was born in Long Beach, CA where the U.S. Navy stationed his father at the time.
More articles from Anthony Maddela